Last time we shared with parents how to read blood test report
How much do you remember~
No worry if you don’t. Just check out the link below!
After having a general understanding on the blood test report
let’s go further
and learn how to read the liver function test report
Liver function
Although the parameters in a liver function test report
are not as many as those on the blood test report
they are much more important
for children who just went through a liver transplantation
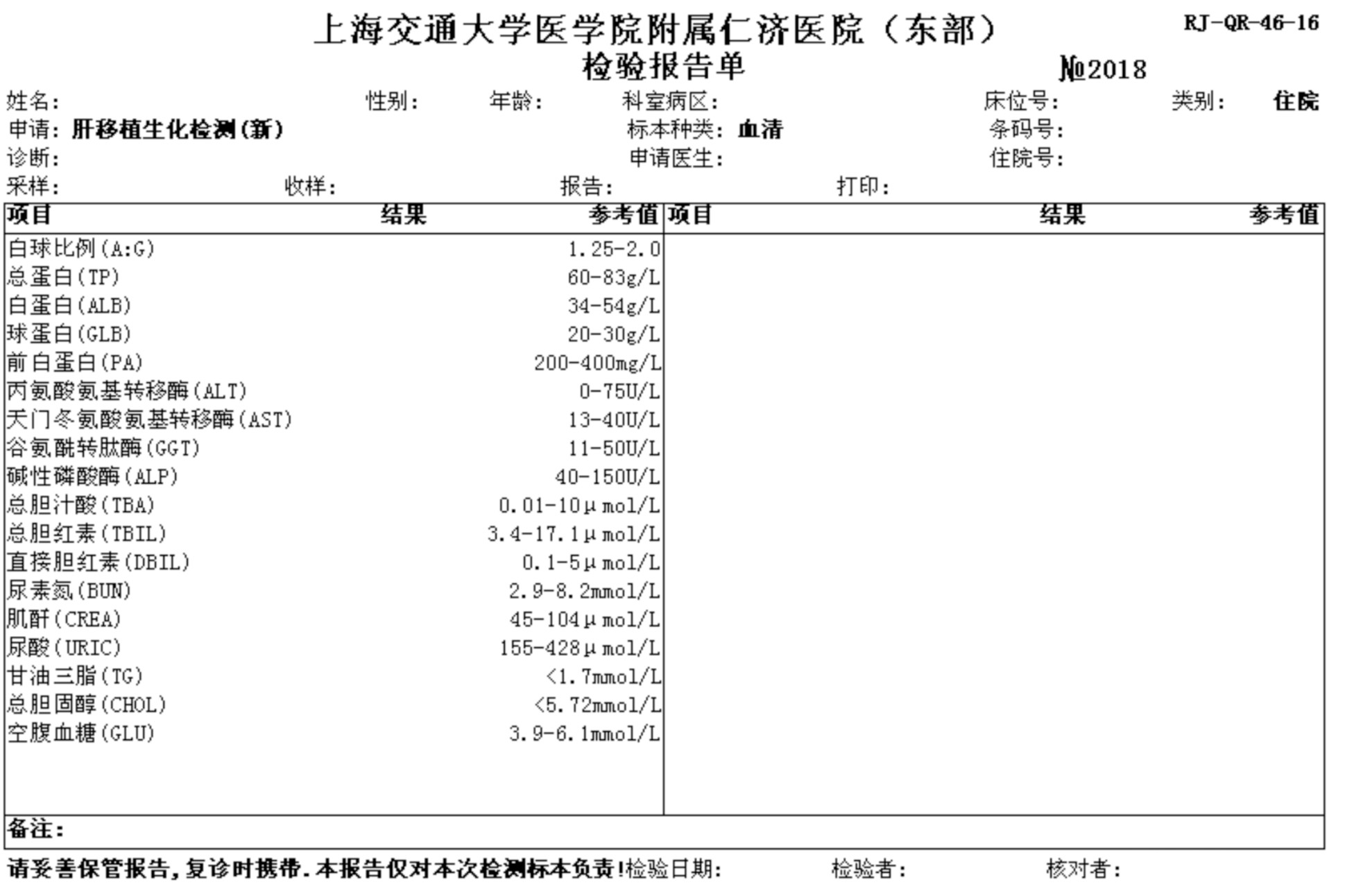
Protein metabolic function
The protein metabolic function test includes: serum total protein (TP), albumin (ALB), globulin (GLB), albumin/globulin ratio (A:G) and prealbumin (PA).
Serum total protein (TP):
↓:Often seen in decrease of protein synthesis (such as poisoning, severe liver injury, etc.), insufficient protein intake (such as nutrition deficiency, malnutrition, etc.), excessive protein loss (such as renal diseases, extensive burn, protein-losing enteropathy, etc.), chronic wasting diseases (such as malignant tumor, hyperthyroidism, etc.) and hemodilution.
↑:Often seen in the increase of protein synthesis (such as multiple myeloma, macroglobulinemia, etc.), hemoconcentration (dehydration), liver cirrhosis (increase in γ-globulins) and chronic infectious diseases (such as autoimmune liver diseases, sepsis, etc.).
Albumin (ALB):
↓:The reason of an ALB decrease is basically the same as the one for decrease in total protein. It is often seen in the decrease of synthesis (severe injury of liver cells), insufficient protein intake, excessive protein loss, hemodilution, etc.
↑:Often seen in hemoconcentration (severe dehydration, insufficient water intake, shock) and Addison’s disease.
Globulin (GLB):
↓:Has less to do with liver diseases and is often seen in congenital immunodeficiency. Using immunosuppressant and antitumor therapy can physiologically decrease GLB in infants under 3 years old with severe advanced liver and kidney diseases.
↑:Albumin will decrease and globulin will increase when hepatic lesion occurs. It is often seen in chronic liver inflammation and liver fibrosis, along with M-proteinemia, autoimmune diseases, extrahepatic chronic inflammation and infection.
Prealbumin (PA):
↓:Often seen in malnutrition, chronic infection, advanced malignant tumor, diseases of the liver and biliary system (such as hepatitis, liver cirrhosis, liver cancer and obstructive jaundice). The decrease of PA can reflect early hepatocellular damage.
↑:Often seen in Hodgkin lymphoma.
Enzyme examination
The liver is the organ with the richest amount of enzyme in the human body. Its pathological state often reduces changes in the serum enzymes concentration. The determination of serum enzymes can reflect some liver diseases and liver function in general.
Enzymes that mainly reflect hepatocellular damage:
Alanine aminotransferase (ALT), aspartate transaminase (AST)
↓:No clinical significance.
↑:Often seen in acute and chronic viral hepatitis (usually AST/ALT < 1 for acute ones and AST/ALT > 1 for chronic ones), non-viral hepatitis, liver cirrhosis (stay normal or increase slightly in quiescent phase, stay normal or increase moderately in active phase and stay normal or lower slightly in terminal phase), liver cell carcinoma, cholestasis (increase slightly or stay normal), etc.
*Since AST is mainly distributed in the heart, followed by livers, skeletal muscles, kidneys and some other tissues, its increase can also be the result of myocardial injuries, muscle injuries, renal infarction, etc.
Enzyme that mainly reflects cholestasis:
Glutamyltranspeptidase (γ-GT or GGT):
↓:No clinical significance.
↑:Often seen in biliary obstructive diseases (such as cholestasis), space-occupying liver lesions (such as primary hepatic carcinoma, etc.; could be reduced after tumor resection but a decrease followed by an increases could suggest a relapse), acute and chronic viral hepatitis (increase slightly and moderately when acute hepatitis happens), liver cirrhosis (stay normal in stable type and increase slightly or moderately in the progressive type), alcoholic liver diseases, pancreatic cancer, etc.
Alkaline phosphatase (ALP):
↓:Only seen in a few severe diseases (such as cardiopulmonary bypass surgery, insufficient protein supply, magnesium deficiency, severe anemia and hypothyroidism) and hepatolenticular degeneration.
↑:Extrahepatic bile duct obstruction (an increase of ALP at early stage can be seen in gallstones, cholecystitis and sclerosing cholangitis), intrahepatic cholestasis (such as cholestatic hepatitis, intrahepatic cholestasis caused by alcohol), focal hepatic lesion (an increase of ALP is more obvious than that of aminotransferase in primary hepatic carcinoma). There might be a physiological increase of ALP in pregnant women and children due to active bone or placental growth.
Bilirubin metabolism
The bilirubin metabolism is closely related to digestion and absorption of lipids and the formation of jaundice. It consists of serum total bilirubin (TBIL), indirect bilirubin (IBIL) and direct bilirubin (DBIL). The value of IBIL is TBIL minus DBIL.
Jaundice and its severity:
Occult (subclinical) jaundice: TBIL 17.1-34.2 μmol/L
Mild jaundice: TBIL 34.2-171 μmol/L
Moderate jaundice: TBIL 171-342 μmol/L
Severe jaundice: TBIL > 342 μmol/L
Determine the cause and type of jaundice:
Hemolytic jaundice: Usually mild jaundice and is mainly caused by the increase of IBIL. Can be seen in various hemolysis, blood transfusion reaction, large hematoma absorption, etc.
Hepatocellular jaundice: Usually is mild to moderate jaundice and is caused by the increase of both DBIL and IBIL. Can be seen in acute and chronic hepatitis, liver cirrhosis, and material injury caused by cholestasis.
Obstructive jaundice: Usually is moderate to severe jaundice and is mainly caused by the increase of DBIL. Can be seen in biliary atresia, cholelithiasis, biliary tract tumor, primary biliary cirrhosis, etc.
*Sometimes the level of serum TBIL and DBIL can be extremely high during the convalescence of hepatitis.
Bile acid metabolism
Detection of serum total bile acid can reflect the synthesis, absorption and excretion of hepatocytes. It is a more sensitive diagnostic parameter for hepatocellular injury and can also reflect lesions in intestinal tract, biliary tract and portal system.
Total bile acid (TBA):
↓:No clinical significance
↑:Often seen in hepatocellular injuries (substantial increase in acute hepatitis, chronic active hepatitis, liver cirrhosis and liver cancer; TBA positive rate can be much higher than other parameters in liver cirrhosis), biliary tract obstruction (cholelithiasis and biliary tumor) and portacaval shunt. A physiological increase of TBA could happen after meals.
